55 11/2005
NASCO (National Account Service Company Operation) is an automated claims
processing system dedicated to the handling of claims for any national account that
specifically contracts to be a part of the (NASCO) system. The Voucher shows how
your patient's claims were processed.
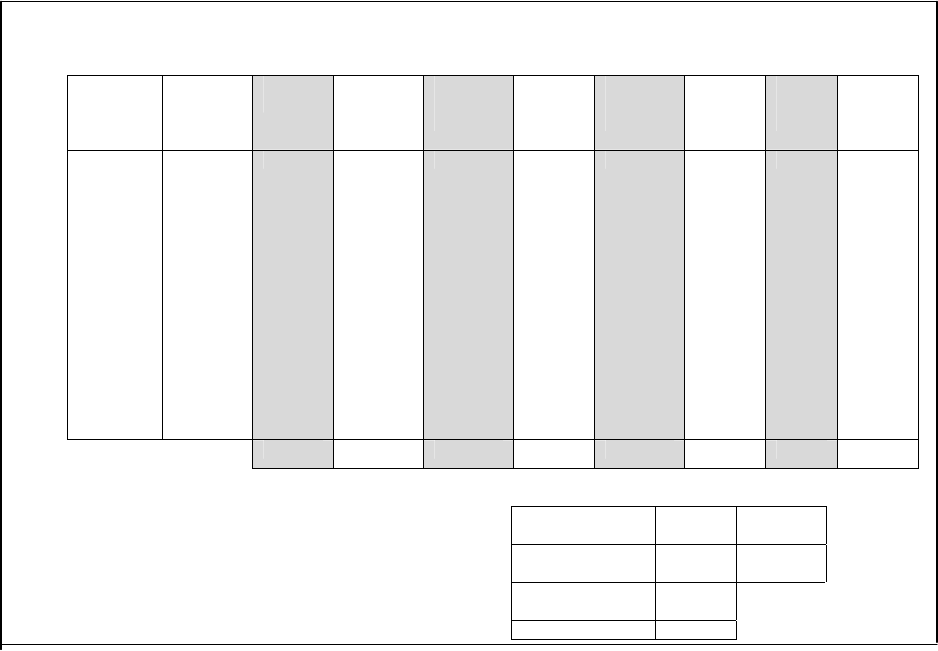
PROVIDER VOUCHER
(1) (2) (3) (4) (5) (6) (7) (8) (9) (10)
SERVICE
DATES
FROM/TO
PROCEDUR
E
CODE
CVD/NCVD
TOTAL
CHARGES
ALLOWED
AMOUNT
OTHER
INSURANCE
DOLLARS
SUBSCRIBE
R
LIABILITY
APPROVE
D
TO PAY
AMOUN
T
PAID
RSN
CODE
(11)
(13)
(12)
(14)
TOTAL
PROVIDER NUMBER TAX ID PAYMENT
DATE
71020000001234 12-
345678
01-02-97
(15)
REFERENCE NUMBER PAGE NO.
12345678912345 1
(1) SERVICE FROM AND TO DATES: The first and last date of service reported for the patient's claim.
(2) PROCEDURE CODE/CVD/NCVD (COVERED DAY/NONCOVERED DAY): Procedure Code identifies the reported code for the specific procedure administered. Covered
day/non-covered day will show the total service days.
(3) TOTAL CHARGES: This column represents your billed amount for the service(s) administered.
(4) ALLOWED AMOUNT: The amount approved for payment prior to member liability.
(5) OTHER INSURANCE DOLLARS: The amount paid by other insurance, including Medicare.
(6) COLUMN 6: This column will be titled either PROVIDER'S LIABILITY or OTHER AMOUNTS NOT COVERED. When titled PROVIDER'S LIABILITY this column will represent
the amount of the provider's liability for the services performed. When titled OTHER AMOUNTS NOT COVERED this column will represent other amounts not covered
for these services.
(7) SUBSCRIBER'S LIABILITY: This column indicates the amount of the patient's liability for the services performed.
(8) APPROVED TO PAY AMOUNT: This column identifies the amount approved for payment after taking into consideration the member's liability.
(9) AMOUNT PAID: The amount paid for the service(s) reported.
(10) REASON CODE: Codes are shown in this column which refer to specific messages below each claim. These messages clarify a payment situation or explain why you
may be responsible for a service.
(11) SUBSCRIBER IDENTIFICATION: The contract number under which the claim was processed.
(12) PATIENT'S NAME: The name of the patient for whom services were performed.
(13) CLAIM #: The number assigned to a patient's claim.
(14) PATIENT ACCT/PRESCRIPTION NUMBER: Your internal patient number. For Pharmacists, the number represents the Prescription Number.
(15) (15) REFERENCE NUMBER: For internal use.


















